Hip pain & "bursitis"... what is going o…
Laura McCrystal
Monday, 18 November 2019
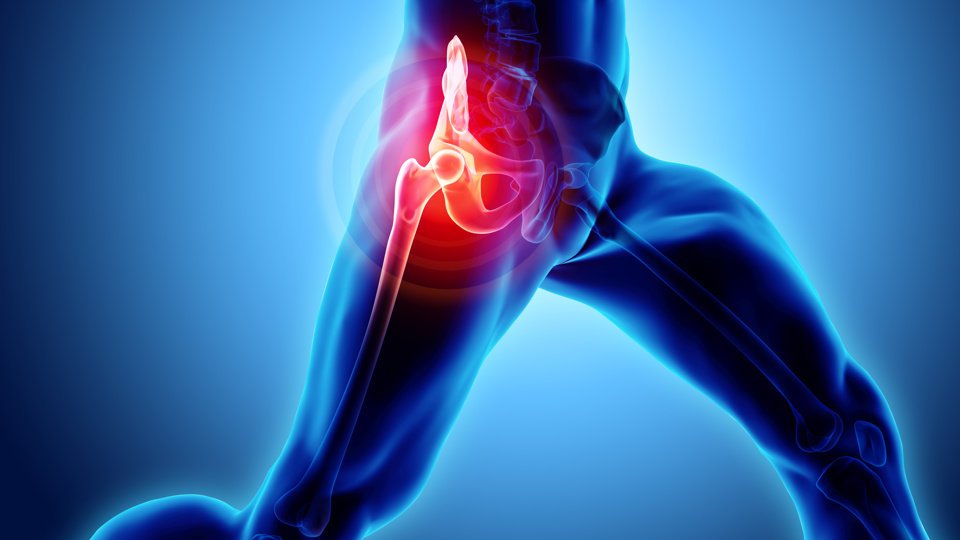
Hip pain & "bursitis"... what is going on & what you can do about it
In this blog our Clinical Specialist Physiotherapist Lauren explores lateral hip and gives you some tips to help settle these symptoms.