Pregnancy Related Pelvic Pain
Pregnancy Related Pelvic Pain
In this blog we explore pelvic pain in pregnancy.

What is Pelvic Girdle Pain?
I assume you’re reading this if you, or a loved one close to you, has started to experience symptoms of pain whilst pregnant. Firstly – congratulations, it will be worth it, I promise! This blog aims to help
you understand what PGP is, why you might be getting these symptoms, and most importantly how to deal with them so that you can focus on enjoying your pregnancy.
Pelvic girdle pain (PGP) is a very common condition, experienced by around 1 in 5 pregnant women. It was formerly known as SPD (symphysis pubis dysfunction), although this term is outdated as we
now know that it affects many more structures than just the symphysis pubis – extra points if you even know where that is!
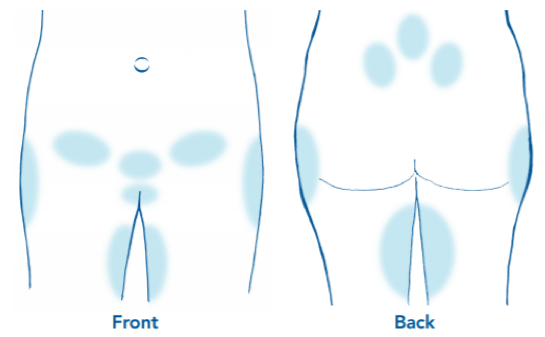
It is also a very individual condition; most women have different symptoms that can continue to change throughout the course of pregnancy. It may be reassuring to know that the pain experienced
in PGP can be very unpredictable; some days can be really good, others can be agony, seemingly for no reason. The pain can be one sided, or both sides, and has a habit of moving around, which can make you worry about what is going on - rest assured, this is normal! If this resonates with you, and you have pain in any of the shaded areas below, it is highly likely that you are experiencing PGP.
Who Gets PGP?
You may have already read about the hormone called Relaxin, released from week 2 of conception, which gets a lot of the blame for causing the pain. However, research has shown us
that the levels of Relaxin in women who experience PGP compared to those who don’t are actually no different, so this is not even close to the full story. It affects ALL ages, ALL shapes and sizes, and can happen in the first, second or third trimester. Sometimes, women have no risk factors at all.
However, there are several risk factors, often individual to you. These include, but are not limited to:
- Previous history of back or pelvic pain (especially during a previous pregnancy)
- Weight
- Fitness levels (including recent/historical/pre-pregnancy injuries)
- Occupational demands and daily activities
- Postural habits
- Hypermobility
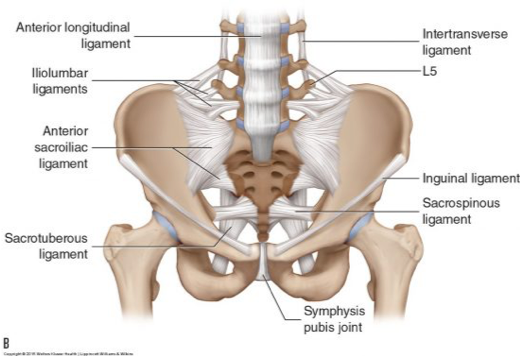
To understand why this condition is commonly very painful, we must first understand how important the role of the pelvis is in everyday life. The pelvis is our base of support; it transmits everything our lower body does up into our trunk, and every upper body and spinal movement down into our legs.
It absorbs a lot of our impact throughout the day, and in a “normal” (read: NON-PREGNANT) pelvis, it generally does this without any discomfort whatsoever. It is tightly bound together by many ligaments, whose main job is to limit movement, providing a lovely stable platform for your spine.
Is PGP Normal?
“Normally” (read: when you aren’t growing a small human inside you) the pelvic ligaments allow a maximum of about 4mm of movement – not much at all! But then throw Relaxin PLUS a growing baby into the mix, and all of a sudden the job of your pelvis has completely changed.
It has to adapt to huge changes in posture and load in a relatively short space of time, with significantly less stability than it had before. This also changes the demands on the muscles and other soft tissues that act around your pelvis, and this is often one of the biggest contributing factors to why the pain develops. Some women cope with these changes better than others, and more often than not this is dependent on your risk factors above!
I want to be very clear: PGP does NOT worsen simply because you become more pregnant. There are always things you can do to manage the symptoms, no matter how early or developed your pregnancy is. Sometimes, it will go away on its own with a few simple, consistent strategies. Most commonly, the overall level of pain will reduce to become less severe AND less frequent if the same simple and consistent strategies are applied.
The most important thing you can do is speak to your midwife, GP or physiotherapist as soon as you start to experience symptoms. Although common, PGP is NOT normal (similar to pelvic floor dysfunction, but more on that later) and should not be dismissed with the answer “oh – sounds like the normal aches and pains of pregnancy”.
Just as there is no single CAUSE of PGP, there can be no single CURE either. It is very important you learn to understand your symptoms so that you can manage them better. Often the only way to do this is to talk it through with a qualified health professional, as we can find things you are doing that may be making your pain worse, that you won’t even have considered before! Our job is to help your body to slowly adapt to the changes it is experiencing, address the underlying issues to keep you comfortable and come out of your pregnancy feeling stronger, wiser and ready to take care of a newborn baby.
If you haven’t already, an absolute must-read and fantastic resource has been published by the professional network of Pelvic Obstetric and Gynaecological Physiotherapists, and you can access this free of charge HERE. There is a comprehensive lists of DO’s and DON’T’s, advice about management and what physiotherapy can offer someone with PGP. However, it has to be generic; I want to expand on a few more points that this booklet so helpfully makes.
What Makes the Pain Worse?
The most provocative causes of PGP seem to be single-legged/hip dominant activities, including:
- Stairs
- Standing on one leg (think about how you’d normally dress your lower body, or stand in a queue)
- Turning over in bed, getting in/out of bed, lying on one side in bed (come to think of it, anything you do in bed…)
- Getting in/out of a car
- Getting in/out of the bath
- Sitting with your legs/ankles crossed (cue you to quickly uncross them upon reading this)
- Certain forms of exercise may not be helpful
There are SO many habits you may start to notice your pelvis is not to coping so well with. It is generally understood that these single-leg activities are the most painful because they require the pelvis to do a fair bit of work distributing the forces, and it will really struggle to do this through one side. Wherever possible, aim to MODIFY your single-leg activities to double-leg ones, so they don’t aggravate your pelvis as much. Sounds simple right?
In part two will give you some tips on how to modify your activity and some exercises you can do to help ease the symptoms. We are happy to talk to you about your symptoms you can contact us at 01788331570 or email admin@lmcphysio.co.uk. Alternatively you can book an appointment with our Womens Health Physio Lauren Williams here.
See you next week for Part 2.